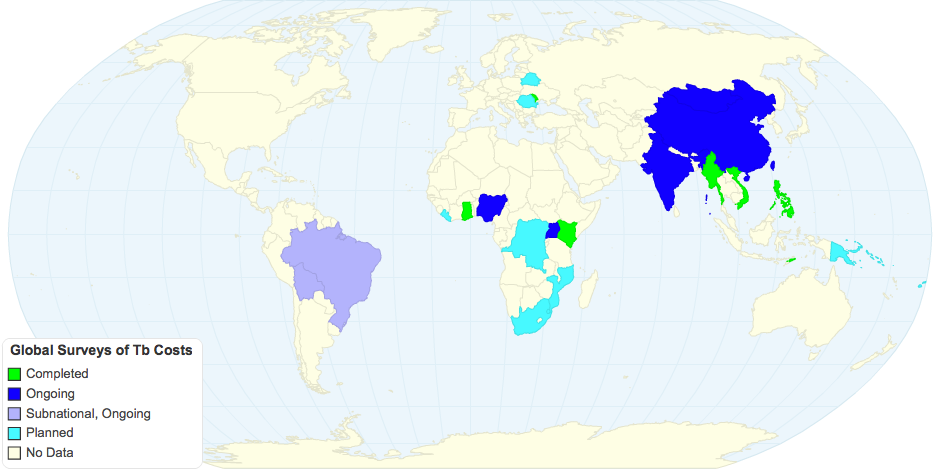
The map reflects completed, ongoing, subnational-ongoing*[4], and planned WHO surveys for patient costs associated with TB illness and treatment. Patient cost surveys are necessary to determine the proportion of households in each country experiencing "catastrophic costs" due to TB illness and treatment. Catastrophic costs are defined as a loss of over 20% of a household's annual income, due to TB[1,2,3,4]. This is measured through "direct costs" like medicine, transport to healthcare, and extra food or care necessary for patients, in addition to "indirect costs", such as loss of work/income, selling assets, or borrowing from family or friends.
A major tenet of the WHO's "End TB" Strategy is to bring the proportion of households experiencing catastrophic TB costs to 0% by 2020, and to maintain 0% at every five-year benchmark until 2035[3,4]. However, data from nations where surveys have been completed, alongside observational epidemiological studies, demonstrate a high prevalence of households with catastrophic costs (e.g. 63% in Viet Nam[4], 65% in Myanmar[3], and 39% in Lima, Peru[1]). Importantly, catastrophic costs are linked with worse socioeconomic and clinical outcomes[1,2]. In other words, catastrophic costs due TB push people further into poverty and increase adverse health outcomes like death, failure of the treatment regimen to cure TB, and defaulting TB treatment.
These data demonstrate that we must amend the third goal of the End TB strategy concerning catastrophic costs. Necessary is more focus upon key risk factors of these costs to identify those most at risk–and to link these households with social protection programs and treatment options that will improve health outcomes and decrease community transmission of TB.
*Subnational surveys are being conducted in São Paulo, Brazil and Cochabamba, Bolivia.[4]
Literature Cited:
[1]Wingfield T, Boccia D, Tovar M, Gavino A, Zevallos K, Montoya R, et al. Defining catastrophic costs and comparing their importance for adverse tuberculosis outcome with multi-drug resistance: a prospective cohort study, Peru. PLoS Med (2014)11:7:e1001675
[2]Wingfield T, Tovar MA, Huff D, Boccia D, Saunders MJ, et al. Beyond pills and tests: addressing the social determinants of tuberculosis. Clinical Medicine (2016)16:6:s79-s91.
[3]WHO. Global tuberculosis report 2016. Geneva: World Health Organization, 2016.
[4]WHO. Global tuberculosis report 2017. Geneva: World Health Organization, 2017.
8 years ago